Sleep Apnea
What is it? And could you have it?
It's called obstructive sleep apnea (OSA), and it's estimated that more than 18 million Americans share this problem. Even more alarming, it's estimated that only one in ten of these individuals has been diagnosed with this OSA.
Chances are you are reading this now because you or your doctor believes your symptoms suggest the possibility of OSA.
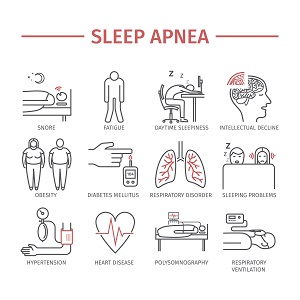
There are many reasons why it's important to diagnose OSA and start therapy without delay. Left untreated, OSA can significantly increase your risk of developing high blood pressure or experiencing a heart attack or stroke. Other conditions could result from untreated OSA, including diabetes and memory loss.
What is obstructive sleep apnea?
 OSA is caused by a physical narrowing or collapse of the upper part of the air passage, behind the tongue, during sleep that interrupts breathing and inhibits or prevents air from getting into your lungs.
OSA is caused by a physical narrowing or collapse of the upper part of the air passage, behind the tongue, during sleep that interrupts breathing and inhibits or prevents air from getting into your lungs.
As you fall asleep, the muscles surrounding the air passage begin to relax, partially or fully blocking the air passage. In turn, each breath is forced through a constricted opening that creates a loud, snoring sound.
While this is happening, your heart, brain and other organs are being deprived of oxygen each time breathing is interrupted. Breathing can actually stop for ten seconds or longer while you’re sleeping. If this happens more than 15 times over the course of an hour, then you most likely have OSA.
And if you have hypertension, then you most likely have OSA if breathing stops five times per hour. These interruptions and sudden awakenings that prompt you to breathe again can occur hundreds of times each night – even though you probably won’t remember any of it.
Take this simple test.
Your health and life could depend on it.
EPWORTH SLEEPINESS SCALE©
How likely are you to doze off or fall asleep in the following situations in contrast to just feeling tired? This refers to your usual way of life in recent times. Even if you have not recently done some of these things, try to work out how they would have affected you.
Use the following scale to choose the most appropriate number for each situation:
0 = would never doze or sleep
1 = slight chance of dozing or sleeping
2 = moderate chance of dozing or sleeping
3 = high chance of dozing or sleeping
| Situation | Chance of Dozing or Sleeping | |||
|---|---|---|---|---|
| 0 | 1 | 2 | 3 | |
| Sitting and reading | ||||
| Watching TV | ||||
| Sitting inactive in a public place | ||||
| Being a passenger in a motor vehicle for an hour or more | ||||
| Lying down in the afternoon | ||||
| Sitting and talking to someone | ||||
| Quietly sitting after lunch (No alcohol) | ||||
| Stopped for a few minutes in traffic while driving | ||||
| Epworth Score:0 | ||||
0-9 = Average score, normal population
9+ = Immediately consult your physician
Epworth Sleepiness Scale reprinted with permission of the Associated Professional Sleep Societies (Johns MW; A New Method for Measuring Daytime Sleepiness: The Epworth Sleepiness Scale. SLEEP 1991;14(6):540-545).
How does OSA make you feel?
As you can imagine if you wake up at night choking or gasping for breath, you'll rarely fall into a deep, restful sleep. In turn, it's virtually impossible to wake up feeling fully refreshed. You may feel drowsy and irritable the rest of the day even though you got what you thought was eight or more hours of sleep. (Plus, your snoring may also keep your bed partner awake at night.)
Other signs and symptoms of sleep apnea may include:
Frequent urination during the night
Dry throat when you awake
Coughing
Morning headaches
Memory or learning problems
Mood swings
You may not notice these symptoms yourself, but your bed partner may observe them. Your partner may also be the one who notices that you periodically stop breathing during the night.
Do you have OSA?
Doctors diagnose sleep apnea based on your medical and family histories, a physical exam, and results from a sleep study. Initially, your doctor will ask you and your family questions about how you sleep, and how you function during the day. Your doctor will also perform a physical exam and check your mouth, nose and throat for extra or large tissues.
A physical exam and medical history may be all that’s needed to diagnose your sleep apnea. If your physician thinks you may have OSA, then you’ll be asked to participate in a sleep study for one or two nights at a local hospital, clinic or sleep disorder center. Clinicians will measure a number of vital signs – including oxygen levels – in your blood. A sleep study can help your doctor know for sure, as it is the most accurate test for diagnosing sleep apnea. (Diagnostic devices are now available for in-home sleep studies as well.)
Treating OSA
 There are many methods of treatment suggested by physicians. What works for one individual may not work for another. Success with a certain method often depends on the habits of those involved.
There are many methods of treatment suggested by physicians. What works for one individual may not work for another. Success with a certain method often depends on the habits of those involved.
Most often, continuous positive airway pressure (CPAP) therapy is the treatment of choice by physicians for individuals with OSA. CPAP units are designed to provide a continuous stream of air, through a nasal mask, at a positive pressure, to prevent the air passage from collapsing while you sleep.
Other methods of treatment include:
Losing weight and limiting alcoholic beverages prior to going to bed; excess weight and alcohol both have been shown to make the symptoms of OSA more acute
Sleeping on your side instead of your back to help keep your throat open
Custom-fit oral appliances – these devices have been shown to help some people who have mild sleep apnea
Nasal sprays or allergy medicines to keep your nasal passages open at night
Smoking cessation – symptoms often improve when smokers quit
Restructuring of the soft palate and uvula at the back of the throat; although it is not possible to cure OSA surgically, physicians sometimes recommend this procedure to reduce snoring
What to Expect From CPAP Therapy
Sometimes, it isn't easy to admit you need help, but when your quality of life is at stake, it's important to take that first step towards understanding obstructive sleep apnea (OSA).
Workplace Effects of Sleep Disordered Breathing
Wake Up to the Workplace Effects of Sleep Disordered Breathing